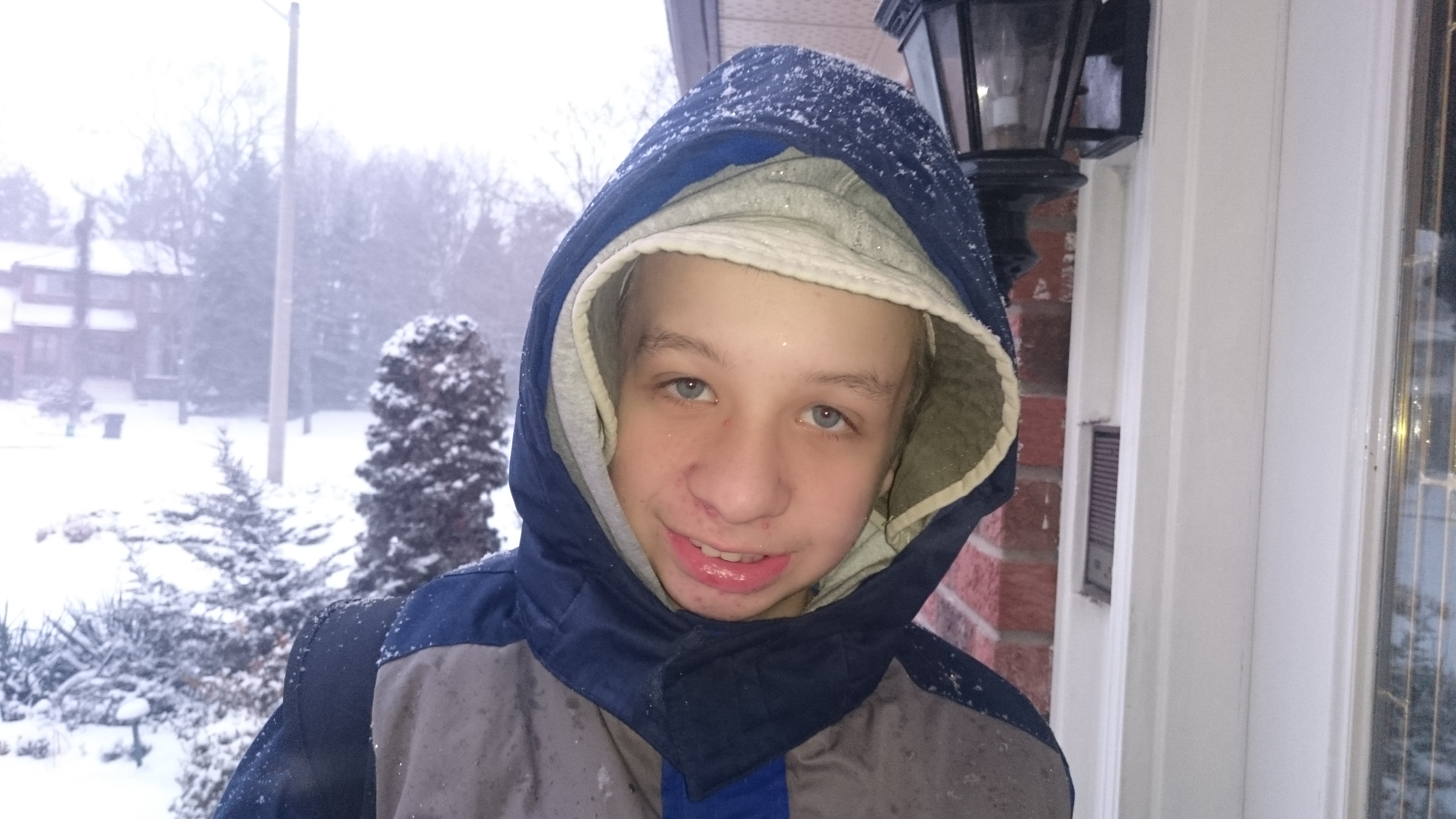
Today’s “Autism Doesn’t End At Five” series features the story of Aaron, who is four years old. Even if he reaches the top of the IBI waitlist before his fifth birthday, which is unlikely, he will only receive services for a short time before his age deems him ineligible.
Aaron was diagnosed with autism when he was just two years old. His mother had done the research: she knew that an early diagnosis followed by early intervention would improve her son’s chances of a good outcome. She was hopeful that now that Aaron had been diagnosed, she would be able to access services for him.
Instead, she found herself and her son being placed onto one waitlist after another. While Aaron is waiting his turn for IBI services, he is missing the developmental window identified by the Ontario government. Now almost four, he still technically qualifies for IBI, but considering that most children spend two years or more on the waitlist, he is unlikely to get to the top of the list by the time he turns five.
Aaron has been identified as being on the severe end of the autism spectrum. He has many challenges: among other things, he is non-verbal, he has limited eye contact, and he is not able to use the toilet independently. Many children have made tremendous gains in all of these areas thanks to IBI therapy.
In spite of his challenges, Aaron has many strengths for IBI service providers to build on. His mother describes him as a “puzzle wizard and builder extraordinaire”. This indicates the presence of strong problem solving skills and solid learning capabilities. Everything points to Aaron being an ideal candidate for IBI, and that is not going to magically change on his fifth birthday.
A year from now, Aaron will still be highly likely to reap enormous benefits from IBI therapy. But a year from now, the Ontario government will cut off his access to this critical therapy simply because of his age.
Aaron’s parents, who also have five-year-old twin girls, are now talking about private therapy. They refuse to give up on their son, but helping him is going to result in upheaval for the family. They are listing their home for sale in an attempt to pay for IBI therapy themselves. No family should have to go through this kind of stress – especially in a country like Canada, which prides itself on human rights and equal opportunities for all people.
“My heart aches for my son and I need to stay strong to be his voice in any way I can.” – Kelly, Aaron’s mother
By Kirsten Doyle. Photo courtesy of Aaron’s mother, Kelly.