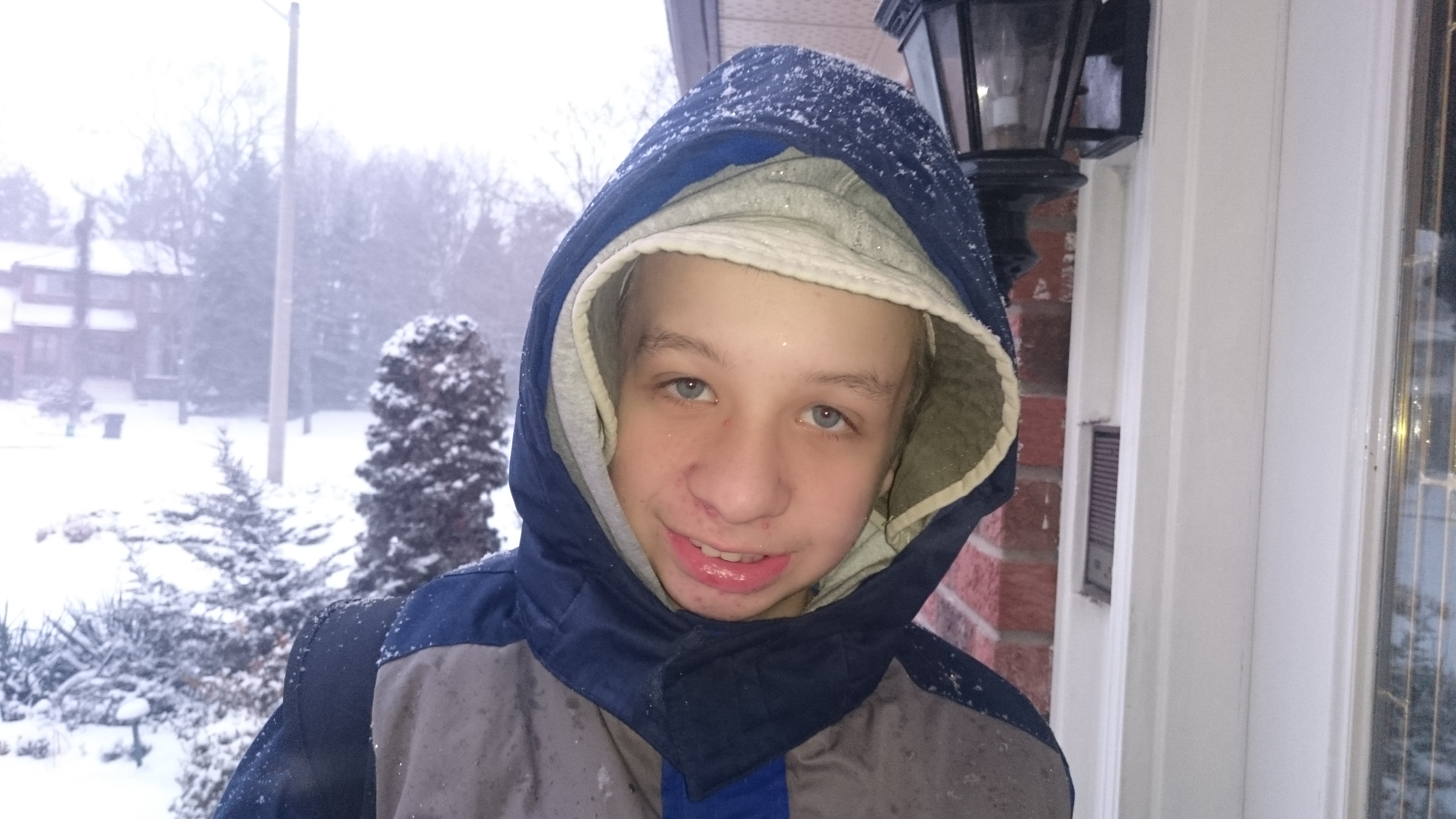
Thirteen years ago I was pregnant. The pregnancy was so new that nobody knew about it apart from me. I remember lying in bed hugging this secret close to me, this secret that I was sharing with no one but the baby growing inside me. I was terrified that my husband and I would experience a repeat of the loss we had been through just a few months previously. Stay with me, I silently begged the baby.
Twelve years ago I was a new mom. I spent time lying on a blanket with my months-old babe, holding his tiny hand in mine. I would look at his little fingers, at the curve of his cheek, and the fluttery eyelashes – and I would marvel at how something so small could be so perfect. I felt as if the future was a blank slate, just waiting to be written by this brand new human being.
Eleven years ago, I was a parent who had recently lost a parent. I held my one-year-old son, feeling immense gratitude that he had spent some time in his grandfather’s arms. I was afraid: when I lost my father, I lost a bit of my security. I somehow became more of an adult, and I wasn’t sure that I was ready for that.
Ten years ago, my little family had gained a new member. As I cared for my newborn baby, I worried about his older brother. I knew that something was not right, but the doctor said, “Wait. Give it some time.” When your instincts say one thing and your doctor says another, you have to decide which one to listen to. I listened to the wrong voice and waited.
Nine years ago, we had finally gotten the doctor to listen, and our firstborn son was on the waiting list for a developmental assessment. We didn’t need an assessment to know that something was wrong, but we were hopeful that whatever it was, it could be fixed. While we waited, we took our son to speech therapy and celebrated every single word that he uttered.
Eight years ago, my husband and I were trying to settle into our roles as autism parents. The initial shock of the diagnosis had worn off, and we were working our way through the labyrinth of government funding and services. At the same time, we were adjusting our dreams and goals to fit the new reality of autism.
Seven years ago, our autism boy was about to start his ABA therapy. It was a world that was completely unknown to us, a form of intervention that works for some kids but not others. Would it work for our boy? We had no way of knowing. A further assessment put him on the severe end of the autism spectrum, but we were urged not to lose hope.
Six years ago, we were one year into the ABA therapy, and we had seen our son make phenomenal progress. His vocabulary had exploded and we were starting to see the emergence of some amazing qualities. A follow-up assessment showed that he had made 23 months’ worth of gains in a 12-month period. Hope sprang eternal.
Five years ago, the boy was slowly, slowly being phased out of ABA therapy and into full-time school. We worried about whether the cessation of therapy would stall the progress we had seen him make. We were advised to expect a temporary plateau followed by slow but steady progress. Anything could happen, we were told. A full decade of school remained. A lot can happen in ten years. I held onto my rose-coloured glasses.
Four years ago, I suffered a devastating loss when my beloved aunt died in a freak accident. For the first time since the death of my father, I had to go away without my family. Leaving my husband and boys was excruciating, but I knew that I was needed on the other side of the world. The autism boy coped well with this big upheaval, helped enormously by his incredible little brother.
Three years ago, my stubborn optimism started to give way to realism. Yes, my son had many capabilities. He was doing well in his special ed program, and he was able to do things by himself, like get dressed and use the bathroom. He had come a long way since the days of his diagnosis. But there was still a lot that he couldn’t do. For the first time, I started to realize that in all probability, my boy would never attain complete independence.
Two years ago, we had to fight for our boy. The special ed programming at his school did not continue beyond Grade 6, and the placement he was slated for filled us with the horrors. The classroom – indeed, the entire school – was overcrowded and staffed with well-meaning but overwhelmed teachers. As I walked the hallways during my one and only visit, I detected an aura of barely contained hysteria. We were not going to risk the years of progress we had seen. And so, with my son’s principal by our side, we started a long series of meetings with the school board. And once again, we waited.
One year ago, the principal of my son’s school called with the news that the battle had been won. A special ed program for Grade 7 and 8 kids was being brought into his school – a school where the general student body forms a protective and loving wall around the special ed kids. I cried with joy, not only for my son, who was getting another two years in this amazing environment, but for all of the kids whose paths we had had a part in altering for the better.
Today, my son is in Grade 7, in his first year of the newly implemented program. He is doing well and continuing to make progress. I am happy with where he is, but I am afraid of where he is going. Because unlike the day of his diagnosis, when we had years of time ahead of us, we are now very close to the future we talked about then.
One year from now, the boy will be months away from finally leaving the security of the only school he has ever known. We do not know where he will be going for high school – that chapter of the story is starting to be written now. In the next few months – a full year ahead of when this would happen for typical kids – we will be starting to visit high schools, interview principals, look at special ed programs.
This year, next year, and for the rest of our lives, we will continue to do the best thing for our autism boy, to give him the opportunities he needs to reach his full potential – whatever that potential turns out to be.
This is an original post by Kirsten Doyle. Photo credit to the author.